Data and research
Information on all newly diagnosed cases of notifiable STIs and BBVs is collected on standard forms which include questions which ask about the probable mode of transmission, country of birth, and Indigenous status.
This information is forwarded to state/territory health departments – without the names of the people who have been diagnosed, just a code for each case. This is known as surveillance – the monitoring of notifiable disease data.
Surveillance data are sent to the Kirby Institute, which produces annual surveillance reports, including Blood-borne viral and sexually transmitted infections in Aboriginal and Torres Strait Islander people: Annual Surveillance Report. These annual reports show the number of new diagnoses in the previous calendar year, statistics on modes of transmission (e.g., anal sex, heterosexual sex, sharing of injecting drug equipment), and rates of STIs and BBVs. Access the 2018 surveillance report here. [PDF:12.3MB]
For an overview of the 2019 data on HIV rates among Aboriginal & Torres Strait Islander people and a discussion of the growing divergence between rates for Indigenous and non-Indigenous Australians, see HIV and Aboriginal & Torres Strait Islander Communities in 2019, a booklet produced by the South Australian Health and Medical Research Institute.
Government decisions on investment in STI and BBV prevention, treatment and care are made on the basis of surveillance data, along with findings from research studies and consultations with community advocates.
Multijurisdictional Syphilis Outbreak Working Group communiques
The Multijurisdictional Syphilis Outbreak Group (MJSO) produces surveillance reports (formerly known as communiques) which provide updates on epidemiological data for the syphilis outbreak, and the Group’s activities.
STI and BBV research
Research provides the evidence base for developing prevention and treatment initiatives targeting particular communities. Research is also important for monitoring and evaluating programs. Australian research centres which focus on STI and BBV prevention among Aboriginal and Torres Strait Islander communities include:
- The South Australian Health and Medical Research Institute, in Adelaide, conducts research on STI and HIV prevention in Aboriginal communities and the care of people with HIV, developing prevention and treatment strategies targeting communities, and translating research outcomes into proposals for policy development.
- SAHMRI’s Infection and Immunity Aboriginal Health research group is leading the establishment of the Centre for Research Excellence on Aboriginal Sexual Health and Blood-borne Viruses (CRE-ASH) – a five year National Health and Medical Research Council funded study which will develop a sentinel surveillance network to monitor trends in STI and blood borne virus testing and diagnosis data for the Aboriginal and Torres Strait Islander population.
- The Kirby Institute at the University of NSW, produces annual surveillance reports on HIV, viral hepatitis and STI diagnoses among Aboriginal and Torres Strait Islander people.
- The Centre for Social Research in Health (CSRH), at the University of NSW, publishes the Annual Report on Trends in Behaviour which reports on behavioural and attitudinal data on modes of transmission of HIV, viral hepatitis, and STIs in Australia.
- The Burnet Institute collaborates with the Kirby Institute and the National Serology Reference Laboratory on the ACCESS project (Australian Collaboration for Coordinated Enhanced Sentinel Surveillance of STIs and BBVs). ACCESS is establishing a surveillance system to assist in evaluating interventions designed to control STIs and blood borne viruses, including in Aboriginal and Torres Strait Islander communities.
- The Doherty Institute has collaborated with the Monash Department of Epidemiology and Preventive Medicine to conduct a 20+ year study of more than 2.4 million cases of infectious disease across Australia. The study shows that poverty, living remotely or being Indigenous significantly increases the risk of contracting infectious diseases, including STIs and blood borne viruses.
Research Publications
Here are links to a selection of research publications relevant to STI and BBV prevention, testing and treatment in remote Aboriginal and Torres Strait Islander communities.
Conference Posters
Click to view the pdf
Lobo R, D’Costa B. Forbes L, Ward J. (2019, Sept). Promoting STI/BBV testing in remote Aboriginal Communites: Young Deadly Free resources for clinicians. Poster presented at the 2019 Australasian Sexual Health Conference, Perth.
Incidence and prevalence of STIs/BBVs among Aboriginal people
Changing pattern of sexually transmissible infections and HIV diagnosed in public sexual health services compared with other locations in New South Wales, 2010-14. Bourne C, Lam M, Selvey C, Guy R, Callander D. Sex Health. 2018;15(4):366-369. https://doi.org/10.1071/SH17183
An audit on the management and outcomes of infants at risk of congenital syphilis in the Top End of the Northern Territory, Australia, 2005-2013. Rode NBA, Ryder N, Su JY. Commun Dis Intell. 2018;42. pii: S2209-6051(18)00018-0.
HIV incidence in Indigenous and non-Indigenous populations in Australia: a population-level observational study. Ward J, McManus H, McGregor S, Hawke K, Giele C, Su J, McDonald A, Guy R, Donovan B, Kaldor JM. Lancet HIV. 2018;5(9):PE506-E514. https://doi.org/10.1016/S2352-3018(18)30135-8
Prevalence of chlamydia, gonorrhoea, syphilis and trichomonas in Aboriginal and Torres Strait Islander Australians: a systematic review and meta-analysis. Graham S, Smith LW, Fairley CK, Hocking J. Sex Health. 2016;13(2):99-113. https://doi.org/10.1071/SH15171
Prevalence and Correlates of a Diagnosis of Sexually Transmitted Infection Among Young Aboriginal and Torres Strait Islander People: A National Survey. Ward J, Wand H, Bryant J, Delaney-Thiele D, Worth H, Pitts M, Byron K, Moore, Donovan B, Kaldor JM. Sex Transm Dis. 2016;43(3):177-184. https://doi.org/10.1097/OLQ.0000000000000417
Incidence of curable sexually transmissible infections among adolescents and young adults in remote Australian Aboriginal communities: analysis of longitudinal clinical service data. Silver BJ, Guy RJ, Wand H, Ward J, Rumbold AR, Fairley CK, Donovan B, Maher L, Dyda A, Garton L, Hengel B, Knox J, McGregor S, Taylor-Thomson D, Kaldor JM; STRIVE investigators. Sex Transm Infect. 2015;91(2):135-141. https://doi.org/10.1136/sextrans-2014-051617
Infectious and congenital syphilis notifications associated with an ongoing outbreak in northern Australia. Bright A, Dups J. Commun Dis Intell Q Rep. 2015;40(1):E7–E10.
Population movement can sustain high STI prevalence in remote Australian Indigenous communities. Hui B, Gray R, Wilson D, Ward J, Smith A, Philip D, Hocking J, Regan D. BMC Inf Dis. 2013;13:188. https://doi.org/10.1186/1471-2334-13-188
HIV—risk of concentrated epidemic
“No-one’s driving this bus” – qualitative analysis of PrEP health promotion for Aboriginal and Torres Strait Islander gay and bisexual men. Hope A, Haire B. Australian and New Zealand Journal of Public Health. 2019; 43(1). https://doi.org/10.1111/1753-6405.12852
Priorities for preventing a concentrated HIV epidemic among Aboriginal and Torres Strait Islander Australians. Ward J, Hawke K, Guy R. Med J Aust. 2018;209(1):56. https://doi.org/10.5694/mja17.01071
Low HIV testing rates among people with a sexually transmissible infection diagnosis in remote Aboriginal communities. Ward JS, Dyda A, McGregor S, Rumbold A, Garton L, Donovan B, Kaldor JM, Guy RJ. Med J Aust. 2016;205(4):168-171. https://doi.org/10.5694/mja15.01392
HIV in Saskatchewan merits urgent response. Vogel L. Can Med Assoc J. 2015;187(11):793-794. https://doi.org/10.1503/cmaj.109-5105
So Far, So Good: Maintenance of Prevention is required to Stem HIV Incidence in Aboriginal and Torres Strait Islander Communities in Australia. Ward J, Costello M, Willis J, Saunders M, Shannon C. AIDS Educ Prev. 2014;26(3):267-279. https://doi.org/10.1521/aeap.2014.26.3.267
Risk behaviours / social determinants
The GOANNA Survey 2. Results of the second Australian survey of knowledge, relationships, behaviour and health service access relating to sexually transmissible infections (STIs) and blood borne viruses (BBVs) among Aboriginal and Torres Strait Islander young people. Ward JS, Elliott S, Bryant J, Donovan B, Pitts M, Wand H, Kaldor J. Adelaide: South Australian Health and Medical Research Institute (SAHMRI), 2020. https://youngdeadlyfree.org.au/goanna2/
Setting the record straight: sexually transmissible infections and sexual abuse in Aboriginal and Torres Strait Islander communities. Ward JS, Hengel B, Ah Chee D, Havnen O, Boffa JD. Med J Aust. Feb 2020. https://doi.org/10.5694/mja2.50492
Low education levels are associated with early age of sexual debut, drug use and risky sexual behaviours among young Indigenous Australians. Wand H, Bryant J, Worth H, Pitts M, Kaldor JM, Delaney-Thiele D, Ward J. Sex Health. 2017;15(1):68-75. https://doi.org/10.1071/SH17039
Sexual agency, risk and vulnerability: a scoping review of young Indigenous Australians’ sexual health. Journal of Youth Studies. Bell S, Aggleton P, Ward J, Maher L. 2017;20(9):1208-1224. https://doi.org/10.1080/13676261.2017.1317088
Individual and population level impacts of illicit drug use, sexual risk behaviours on sexually transmitted infections among young Aboriginal and Torres Strait Islander people: results from the GOANNA survey. Wand H, Ward J, Bryant J, Delaney-Thiele D, Worth H, Pitts M, Kaldor JM. BMC Public Health. 2016;16:600. https://doi.org/10.1186/s12889-016-3195-6
Sexual behaviour, drug use and health service use by young Noongar people in Western Australia: a snapshot. Williams R, Lawrence C, Wilkes E, Shipp M, Henry B, Eades S, et al. Sexual Health. 2014;12(3):188-193. https://doi.org/10.1071/SH14038
Illicit and injecting drug use among Australian indigenous young people in urban, regional and remote Australia. Bryant J, Ward J, Wand H, , Bamblett A, Waples-Crowe P, Betts S, Coburn T, Delaney-Thiele D, Worth H, Kaldor J, Pitts M. Drug Alcohol Rev. 2016;35(4):447-455. https://doi.org/10.1111/dar.12320
Methods of a national survey of young Aboriginal and Torres Strait Islander people regarding sexually transmissible infections and bloodborne viruses. Ward J, Bryant J, Wand H, Kaldor J, Delaney-Thiele D, Worth H, Betts S, Waples-Crowe P, Cairnduff S, Coburn T, Donovan B, Pitts M. Aust N Z J Public Health. 2016;40(Suppl 1):S96-S101. https://doi.org/10.1111/1753-6405.12427
Sexual risk and healthcare seeking behaviour in young Aboriginal and Torres Strait Islander people in North Queensland. Scott R, Foster R, Oliver LN, Olsen A, Mooney-Somers J, Mathers B, Micallef JM, Kaldor J, Maher L. Sex Health. 2015;12(3):194-199. https://doi.org/10.1071/SH14092
Sexual Health and relationships in young Aboriginal and Torres Strait Islander people: Results from the first national study assessing knowledge, risk practices and health service use in relation to sexually transmitted infections and blood borne viruses. Ward J, Bryant J, Wand H, Pitts M, Smith A, Delaney-Thiele D, et al. Alice Springs: Baker IDI Heart & Diabetes Institute, 2014.
Testing and treatment—service issues
Young Aboriginal people’s engagement with STI testing in the Northern Territory, Australia. Bell S, Aggleton P, Ward J, Murray W, Silver B, Lockyer A, Ferguson T, Fairley CK, Whiley D, Ryder N, Donovan B, Guy R, Kaldor J, Maher L. BMC Public Health. 2020; 20:459. https://doi.org/10.1186/s12889-020-08565-0
Global Epidemiologic Characteristics of Sexually Transmitted Infections Among Individuals Using Preexposure Prophylaxis for the Prevention of HIV Infection: A Systematic Review and Meta-analysis. Ong JJ, Baggaley RC, Wi TE, et al. JAMA Netw Open. 2019;2(12):e1917134. https://doi.org/10.1001/jamanetworkopen.2019.17134
Qualitative perspectives on the sustainability of sexual health continuous quality improvement in clinics serving remote Aboriginal communities in Australia. Gunaratnam P, Schierhout G, Brands J, Maher L, Bailie R, Ward J, Guy R, Rumbold A, Ryder N, Fairley C, Donovan B, Moore L, Kaldor J, Bell S. BMJ Open. 2019;9:e026679. https://doi.org/10.1136/bmjopen-2018-026679
Molecular point-of-care testing for chlamydia and gonorrhoea in Indigenous Australians attending remote primary health services (TTANGO): a cluster-randomised, controlled, crossover trial. Guy RJ, Ward J, Causer LM, Natoli L, Badman SG, Tangey A, Hengel B, Wand H, Whiley D, Tabrizi SN, Shephard M, Fairley CK, Donovan B, Anderson DA, Regan DG, Maher L, Kaldor JM. Lancet Infect Dis. 2018;18(10):1117-1126. https://doi.org/10.1016/S1473-3099(18)30429-8
Molecular test for chlamydia and gonorrhoea used at point of care in remote primary healthcare settings: a diagnostic test evaluation. Causer LM, Guy RJ, Tabrizi SN, Whiley DM, Speers DJ, Ward J, Tangey A, Badman SG, Hengel B, Natoli LJ, Anderson DA, Wand H, Wilson D, Regan DG, Shephard M, Donovan B, Fairley CK, Kaldor JM. Sex Transm Infect. 2018;94(5):340-345. https://doi.org/10.1136/sextrans-2017-053443
Patient staffing and health centre factors associated with annual testing for sexually transmissible infections in remote primary health centres. Hengel B, Wand H, Ward J, Rumbold A, Garton L, Taylor-Thomson D, Silver B, McGregor S, Dyda A, Mein J, Knox J, Maher L, Kaldor J, Guy R. Sex Health. 2017;14(3):274-281. https://doi.org/10.1071/SH16123
Wide variation in sexually transmitted infection testing and counselling at Aboriginal primary health care centres in Australia: analysis of longitudinal continuous quality improvement data. Nattabi B, Matthews V, Bailie J, Rumbold A, Scrimgeour D, Schierhout G, Ward J, Guy R, Kaldor J, Thompson SC, Bailie R. BMC Infect Dis. 2017;17(1):148. https://doi.org/10.1186/s12879-017-2241-z
Development of a Risk Algorithm to Better Target STI Testing and Treatment Among Australian Aboriginal and Torres Strait Islander People. Wand H, Bryant J, Pitts M, Delaney-Thiele D, Kaldor JM, Worth H, Ward J. Arch Sex Behav. 2017;46(7):2145-2156. https://doi.org/10.1007/s10508-017-0958-9
Trends in chlamydia and gonorrhoea testing and positivity in Western Australian Aboriginal and non-Aboriginal women 2001-2013: a population-based cohort study. Reekie J, Donovan B, Guy R, Hocking JS, Kaldor JM, Mak DB, Pearson S, Preen D, Wand H, Ward J, Liu B. Sex Health. 2017;14(6):574-580. https://doi.org/10.1071/SH16207
Why are men less tested for sexually transmitted infections in remote Australian Indigenous communities? A mixed-methods study. Su JY, Belton S, Ryder N. Cult Health Sex. 2016;18(10):1150-1164. https://doi.org/10.1080/13691058.2016.1175028
Low HIV testing rates among people with a sexually transmissible infection diagnosis in remote Aboriginal communities. Ward JS, Dyda A, McGregor S, Rumbold A, Garton L, Donovan B, Kaldor JM, Guy RJ. Med J Aust. 2016;205(4):168-171. https://doi.org/10.5694/mja15.01392
Addressing structural challenges for the sexual health and well-being of Indigenous women in Australia. Arabena K. Sex Transm Infect. 2016;92(2):88-89. https://doi.org/10.1136/sextrans-2015-052412
Quality improvement interventions for improving the detection and management of curable sexually transmitted infections in primary care (Protocol). Nattabi B, Gudka S, Ward J, Rumbold A. Cochrane Database of Systematic Reviews 2016, Issue 10. Art. No.: CD012374. https://doi.org/10.1002/14651858.CD012374
Early presentation of symptomatic individuals is critical in controlling sexually transmissible infections. Fairley CK, Chow EP, Hocking JS. Sex Health. 2015;12(3):181-182. https://doi.org/10.1071/SH15036
A sexual health quality improvement program (SHIMMER) triples chlamydia and gonorrhoea testing rates among young people attending Aboriginal primary health care services in Australia. Graham S, Guy RJ, Wand HC, Kaldor JM, Donovan B, Knox J, McCowen D, Bullen P, Booker J, O’Brien C, Garrett K, Ward JS. BMC Infect Dis. 2015;15:370. https://doi.org/10.1186/s12879-015-1107-5
Incidence and predictors of annual chlamydia testing among 15-29 year olds attending Aboriginal primary health care services in New South Wales, Australia. Graham S, Guy RJ, Ward JS, Kaldor J, Donovan B, Knox J, McCowen D, Bullen P, Booker J, O’Brien C, Garrett K, Wand HC. BMC Health Serv Res. 2015;15:437. https://doi.org/10.1186/s12913-015-1116-5
Attendance patterns and chlamydia and gonorrhoea testing among young people in Aboriginal primary health centres in New South Wales, Australia. Graham S, Wand HC, Ward JS, Knox J, McCowen D, Bullen P, Booker J, O’Brien C, Garrett K, Donovan B, Kaldor J, Guy RJ. Sex Health. 2015;12(5):445-452. https://doi.org/10.1071/SH15007
Reasons for delays in treatment of bacterial sexually transmissible infections in remote Aboriginal communities in Australia: a qualitative study of health centre staff. Hengel B, Maher L, Garton L, Ward J, Rumbold A, Taylor-Thomson D, Silver B, McGregor S, Dyda A, Knox J, Kaldor J, Guy R, Strive Investigators OB. Sex Health. 2015;12(4):341-347. https://doi.org/10.1071/SH14240
Barriers and facilitators of sexually transmissible infection testing in remote Australian Aboriginal communities: results from the Sexually Transmitted Infections in Remote Communities, Improved and Enhanced Primary Health Care (STRIVE) Study. Hengel B, Guy R, Garton L, Ward J, Rumbold A, Taylor-Thomson D, Silver B, McGregor S, Dyda A, Knox J, Kaldor J, Maher L. Sex Health. 2015;12(1):4-12. https://doi.org/10.1071/SH14080
Factors affecting the quality of antenatal care provided to remote dwelling Aboriginal women in northern Australia. Bar-Zeev S, Barclay L, Kruske S, Kildea S. Midwifery. 2014;30(3):289-296. https://doi.org/10.1016/j.midw.2013.04.009
‘Closing the Gap’: How maternity services can contribute to reducing poor maternal infant health outcomes for Aboriginal and Torres Strait Islander women. Kildea S, Kruske S, Barclay L, Tracy S. Rural and Remote Health. 2010;10(3):1383. Available: www.rrh.org.au/journal/article/1383
Census Data
The Australian Bureau of Statistics’ (ABS) 2016 Data Summary provides a snapshot of 2016 census data for Aboriginal and Torres Strait Islander respondents, including on state/territory of residence.
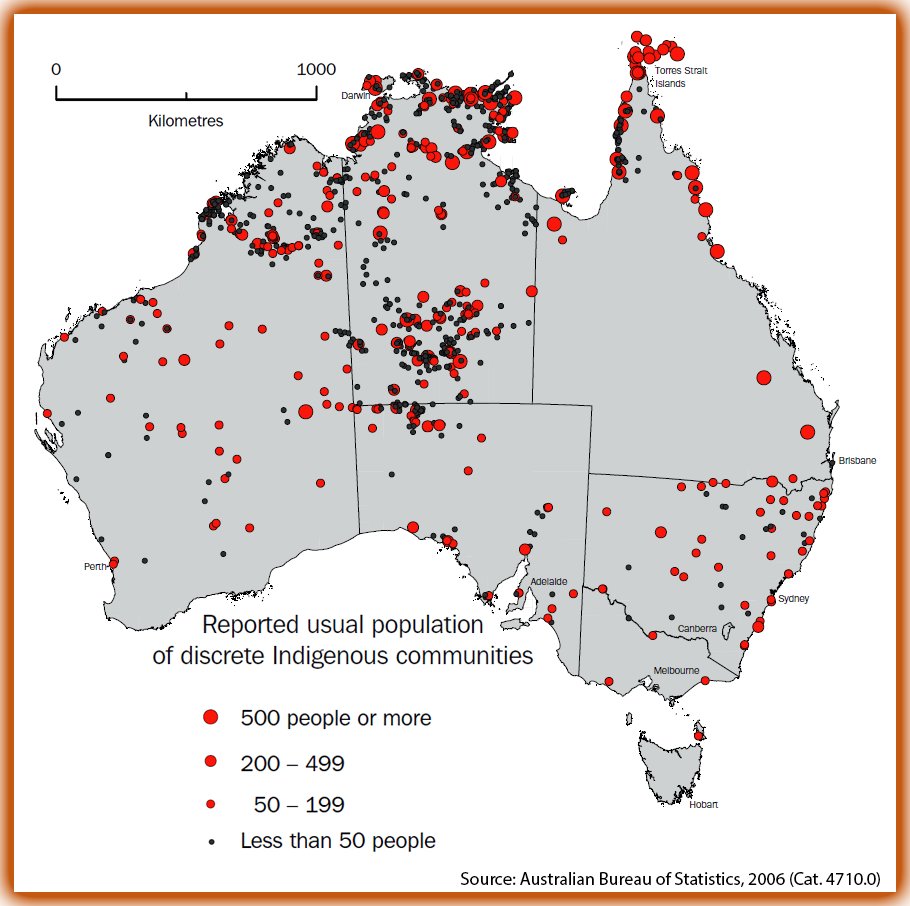
The map graphic below, drawn from 2006 ABS data, shows population density for discrete Aboriginal and Torres Strait Islander communities.
Discrete Indigenous Communities by Usual Population – ABS, 2006 census data